Degenerative-dystrophic diseases of the spine or, more simply, osteochondrosis, not only affect an increasing number of the adult population of our planet, but also become much younger. Today, more than 80% of the working-age population of our planet occasionally suffers from back pain.
Osteochondrosis- spine disease, which results in degenerative-dystrophic damage to the intervertebral discs and lower bone tissue, followed by thickening of the vertebral process and loss of elasticity of the ligaments along the spine. This leads to aging, dehydration and loss of stability in the cartilage tissue.
Osteochondrosis is not only a manifestation of pain in the spine or weakened sensitivity of the limbs, it is a disease of the whole organism. And as many studies prove, osteochondrosis has a direct effect on almost all internal organs. For example, disorders of the cervical spine affect the functioning of the organs of sight, hearing, mental and mental activity. In the thoracic region, they disrupt the work of the cardiovascular system, the gastrointestinal tract. And degenerative-dystrophic changes in the lumbar spine lead to problems with the pelvic organs, including the urogenital area and lower extremities. For example, on the same lower extremities, it is accompanied by various pains, muscle cramps, "creeping", numbness of the extremities, and then their atrophy. Therefore, early detection and qualified treatment of this pathology is very important. Many people who are first diagnosed with an intervertebral hernia are faced with a choice of treatment methods. The proposal for surgical treatment puts many in a state of shock, forcing them to seek alternative therapies. Some immediately turn to traditional healers, bone setters, others take various medications, still others do nothing at all, holding the view that the disease should be treated when it is very worrying. In this regard, there is a winged expression of a neurosurgeon - "walking with a hernia is like walking with a grenade, no one knows when it will explode! " But, unfortunately, surgical treatment, whether neurosurgical or orthopedic, is not a panacea. In many patients, even after surgery, back pain persists, associated with the development of cicatricial adhesions, and recurrences often occur (new worsening ("return") of the disease after apparent recovery) - recurrent hernias.
Osteochondrosis most often affects the intervertebral discs. These unique cartilage washers don’t just connect our 33 vertebrae to the spine. Its good working condition, mobility, elasticity, resilience, ability to withstand the load directly depend on the condition of the intervertebral discs. They serve as spring shock absorbers to relieve the load.
Osteochondrosis is manifested already in the first decades of life and, according to observations, more often in boys than in girls.
If you do not deal with the prevention and treatment of osteochondrosis, the disease will progress, gradually affecting the entire spine, which can ultimately lead to herniated discs, constriction of nerve endings and parts of the spinal cord. In severe cases, the consequences of osteochondrosis can be removed only by surgery with a long period of recovery and rehabilitation.
Types of osteochondrosis
Depending on the part of the spine affected by the disease, the following types of osteochondrosis are distinguished:
- Cervical osteochondrosisor osteochondrosis of the cervical spine.
- Osteochondrosis of the chestor thoracic spine osteochondrosis.
- Lumbar osteochondrosisor osteochondrosis of the lumbosacral spine.
- Frequent osteochondrosis,this is when the disease spreads to two or three parts of the spine at the same time.
- First:the main symptom of osteochondrosis at this stage is instability, which is manifested in the initial disorders of the spinal disc. I feel bad and uncomfortable.
- Seconds:the main symptom of the second stage of osteochondrosis is a bulging disc. The destruction of the annular fiber begins, the gaps between the vertebrae are reduced, it is possible to constrict the nerve endings with pain syndromes.
- Third:in this stage of osteochondrosis the destruction of the ring occurs with the appearance of intervertebral hernias. The third phase is characterized by significant deformation of the spine.
- Fourth:the last and most severe stage of osteochondrosis. It becomes difficult to move. Every movement leads to acute pain. Occasionally the condition improves and the pain subsides, but this clearly indicates the formation of bone growths. They connect the vertebrae, restricting the ability to move and leading to disability.
Four stages of osteochondrosis development
Symptoms characteristic of osteochondrosis
Patients suffering from osteochondrosis complain of constant aching back pain, which is often accompanied by numbness and pain in the limbs. In the absence of adequate treatment, weight loss and limb atrophy occur. The main symptoms are:
- constant back pain, numbness and limb pain;
- increased pain with sudden movements, physical exertion, lifting weights, coughing and sneezing;
- decreased range of motion, muscle cramps;
- with osteochondrosis of the cervical spine: pain in the arms, shoulders, headaches; possible development of the so-called vertebral artery syndrome, which consists of the following complaints: noise in the head, dizziness, glittering "flies", colored spots in front of the eyes combined with a burning pulsating headache. The cause of vertebral artery syndrome can be its spasm in response to direct irritation of the sympathetic plexus due to bone growths, disc herniation, arthrosis of the intervertebral joint and reflex reaction due to irritation of any spinal receptors. The presence of vertebral artery syndrome may worsen the course of coronary or cardiomuscular pathology, if present;
- in osteochondrosis of the thoracic spine: chest pain (like a "ring" in the chest), in the area of the heart and other internal organs;
- with osteochondrosis of the lumbosacral spine: back pain, radiating to the sacrum, lower extremities, sometimes to the pelvic organs;
- nerve root damage (with herniated intervertebral discs, bone growths, spondylolisthesis, spondyloarthritis): cracking pain and impaired sensitivity, hypotrophy, hypotension, weakness of innervated muscles, decreased reflexes.
Diagnosis of osteochondrosis
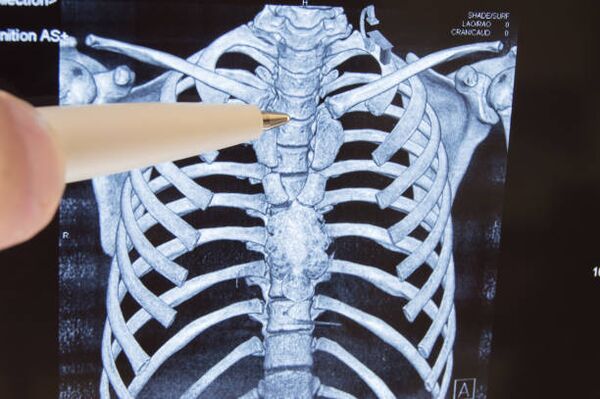
The preliminary diagnosis is made during the initial examination of the patient. The examination is usually performed by a neurologist in connection with the patient's complaints of local changes, which may manifest as pain, deformity, or limited mobility. The spine is examined by the patient standing, sitting and lying down, both at rest and in motion. The level of the spinal lesion is determined by counting the number of vertebrae from certain anatomical landmarks or according to a special scheme.
When examining the back, pay attention to body posture, structural characteristics of the torso, mark the line of spinous growths (middle groove of the back), lower angles of the shoulder blades, ridges of iliac bones, lateral contours of the waist and neck, position of the shoulder girdle, deviation of the intergluteal groove from the vertical. , protrusions of spinous processes pay attention to the relief of the muscles located along the spine.
Spinal sensation allows you to supplement the examination data (presence or absence of deformity) to determine the location, degree and nature of the pain. Palpation also shows tension in the muscles located along the spine. most spinal injuries and diseases are accompanied by increased muscle tone.
Spinal flexion is used to determine the range of motion in different parts of the spine.
The main role in the study of the spine is assigned to radiography, computed tomography and magnetic resonance imaging, with the help of which the level of the lesion is determined, diagnosed and clarified and concretized, and hidden pathologies are discovered. Diagnostic data allow the attending physician to determine treatment tactics and select the most effective treatment methods.
Osteochondrosis of the spine, movement therapy
Complex conservative treatment includes physiotherapy exercises, physiotherapy, massage, manual therapy, traction (traction) of the spine, reflexology, drug therapy.
Physiotherapy exercises (exercise) - the main method of conservative treatment of diseases of the musculoskeletal system, is the creation of dosed loads aimed at decompression of nerve roots, correction and strengthening of the muscular corset, increasing volume and developing a certain stereotype of movement and proper posture, giving ligamentous muscle, as well as to prevent complications. This is achieved through regular exercises with rehabilitation equipment and joint gymnastics. As a result of the exercise, blood circulation improves, the metabolism and nutrition of the intervertebral discs are normalized, the intervertebral space is increased, a muscular corset is formed and the load on the spine is reduced.
Physiotherapy is a method of treatment that uses physical factors: low frequency currents, magnetic fields, ultrasound, laser, etc. It is used to relieve pain, inflammation, rehabilitation after injuries and surgeries. The use of physiotherapy methods shortens the treatment time of many diseases, increases the efficiency of drug use and reduces their dose, there are no side effects inherent in drug treatment.
Massage is a set of methods of mechanical measured action in the form of friction, pressure, vibration, which are performed by hand on the surface of the human body. Effectively relieves muscle tension, muscle pain, improves blood circulation, has a tonic effect.
Manual therapy is a manually adjusted effect on the musculoskeletal system to alleviate acute and chronic pain in the spine and joints, as well as to increase the range of motion and correct posture. One of the directions of manual therapy is visceral manual therapy, which helps restore normal organ mobility, improves blood supply, lymphatic circulation, normalizes metabolism, restores immunity and prevents the worsening of chronic diseases.
Spinal traction (traction) is an effective method of treating pain syndrome in the spine and joints using individually selected loads using special equipment. The procedure is aimed at increasing the intervertebral space, relieving pain and restoring the anatomically correct shape of the spine.
Reflexology - various therapeutic techniques and methods of influencing the reflexogenic zones of the human body and acupuncture points. The use of reflexology in combination with other therapeutic methods significantly increases their efficiency. Reflexology is most often used for osteochondrosis, accompanied by pain, diseases of the nervous system, sleep disorders, mental imbalance, as well as overweight and smoking. By acting on certain points, you can bring the body into harmony and cure many diseases.
Drug therapy is indicated during exacerbation of the disease, is aimed at relieving pain, alleviating the inflammatory process and enhancing metabolic processes by taking or administering drugs by intramuscular or intravenous injection.
Although each of the above methods is highly effective, a lasting therapeutic effect can only be achieved in combination with exercises on rehabilitation equipment, i. when creating a full-fledged muscle corset.
Recommendations for the prevention and prevention of osteochondrosis
To prevent osteochondrosis or reduce pain, people suffering from this disease are advised to stay in a position where the load on the intervertebral discs is minimal for as long as possible, while at the same time stretching the back muscles as often as possible to support metabolicprocesses around the spine. General recommendations come down to following the rules of a healthy lifestyle, in addition, the doctor in any case determines the private recommendations.
The following rules should be followed for prevention:
- Do not overload the spine, do not create conditions conducive to increased pressure on the intervertebral discs:
- limit vertical loads;
- do not make sudden movements, especially body bends when bending;
- avoid falls and jumps from great heights, injuries and bruises of the spine;
- change body position more often;
- keep your back straight;
- try to keep the natural physiological curves of the spine: in the supine position the load on the spine is minimal, but the bed should be semi-rigid (preferably sleeping on a firm orthopedic mattress and orthopedic pillow); in a sitting position keep your back upright because of the muscles or by pressing them against the back of a chair (the chair should be hard enough and the back in a cross section), keep your head upright; in a standing position, change the leg you are leaning on more often; getting out of bed or from a chair, as well as lying down and sitting, should be done with the hands, without straining or bending the back;
- drink water and massage your back before physical activity, it will disperse the blood, speed up metabolic processes and allow the intermittent discs to absorb a sufficient amount of moisture;
- do not lift or hold heavy objects on outstretched arms, to lift the object, squat and then stand up with it, while the objects should be as close to the body as possible;
- when carrying weights, try to distribute the load evenly, that is, do not carry bags in one hand, etc. , if you have to carry an object in front of you, hold it as close to your body as possible and while passing it, do not stretch your arms forward, and use it to carry heavy loads, carts, bags or suitcases on wheels, backpacks;
- when performing heavy work related to lifting, moving or carrying weights, use a wide belt or a special corset;
- do not lift loads over 10 kg;
- when doing any work, try to bend as little as possible and be in a bent position and occasionally unload the spine (hanging on a bar, stretching with arms raised, lying down);
- wear comfortable shoes; women should limit walking in high-heeled shoes.
- Exercise regularly to strengthen and maintain your corset. Swimming is useful.
- Use a contrast shower, soften the body.
- Don't catch a cold.
- Avoid scandals, stressful situations.
- Eat right.
- Don't smoke.



































